Select your baby’s birth date or your due date.
Calendar
Pregnancy
Taking exercise should be part of a pregnant woman’s life. Mild and reinvigorating regular exercise may keep you fit, helping you adjust to the body changes and prevent from hypertension or/and diabetes mellitus. The kind and intensity of exercise should be determined always based on your physician’s consent.
Constipation causes great discomfort to many pregnant women particularly to the ones who suffered from constipation even before pregnancy. A diet rich in liquids and vegetable fibers can eliminate the problem. Hemorrhoids deteriorate or usually make their appearance at an advanced stage of pregnancy and subside or disappear after labor. Lukewarm baths, meticulous hygiene care in the affected area and avoiding the standing position could relieve the symptoms.
However hard it may seem to be pregnant during the summer, keep in mind that these months are and shall remain the most beautiful in your life.
The following tips will help you experience lightly the tough months of summer:
• Keep away from the sun and do not spend much time in suffocating areas that could probably make you faint,
• Have always with you a bottle of water,
• Take lukewarm showers and opt for odorless body lotions with moisturizing texture to avoid any irritation,
• Go for swimming in the morning or in the afternoon,
• Avoid sun exposure, use daily a good sunscreen with a high sun protection factor and always wear a hat,
• In periods of heat wave, ask someone else to do the shopping for you and avoid moving around at least until the sunset,
• Heat combined with the increased weight during pregnancy usually cause discomfort. Try to find time to rest and get some sleep as much as you can to boost your body,
• Prefer loose clothes that do not pressure you,
• Avoid heavy dishes, be careful as to where and what you eat because eating out during the summer is very common.
Stretch marks are a common phenomenon during pregnancy and differ from woman to woman in their number and extent. There are ways to prevent the appearance of stretch marks, such as enough water consumption daily, weight control and hydration using a good moisturizing cream or a combination of moisturizing agents (e.g essential oils) in the areas mostly affected by stretch marks.
- Consume 3-4 meals of fruit and vegetables per day,
- Eat fresh fish preferably twice per week,
- Eat lean red meat (e.g beef) or chicken 2-3 times per week,
- Prefer pulses and dishes cooked with olive oil and vegetables 2-3 times per week,
- Prefer lean meat,
- Avoid fried dishes,
- Wash vegetables meticulously,
- Avoid eating raw or semi-cooked meat,
- Avoid eating raw chicken or eggs due to the risk of contamination from salmonella microbe,
- Avoid eating sweets and sugar in general. If you have an appetite for something sweet, consume fruit or honey but always in moderate quantities,
- Avoid soft drinks as they contain sugar,
- Avoid dairy products of unknown origin, non pasteurized milk and cheese,
- Do not consume sushi and raw fish in general.
Pregnancy normally involves weight gain. Totally a pregnant woman gains 10 to 12 kilos. Most of these kilos should be gained during the 7th, 8th and 9th month, so it is advisable to avoid weight gain during the first months of pregnancy as much as possible.
Total weight distribution stands as follows:
• In the 1st trimester a pregnant woman gains 2 kilos,
• In the 2nd trimester a pregnant woman gains 4 kilos,
• In the 3rd trimester a pregnant woman gains 6 kilos.
The additional weight is due to the increase of the embryos dimensions, the placenta and the quantity of the amniotic fluid. A woman’s adipose tissue quantity increases during pregnancy and the weight of her breasts rises due to the preparation for breastfeeding. The recommendations for weight gain during pregnancy should be individualized based on the Body Mass Index of the mother before the pregnancy (ΒΜΙ = weight/height 2)
It has been calculated that the overall calorie intake during pregnancy is approximately 80.000 calories. Based on the above calculation, the following recommendations were set:
> 150 calories / day above normal intake for the first trimester,
> 350 calories / day above normal intake for the second trimester,
> 350 calories / day above normal intake for the third trimester.
Breastfeeding
Breastfeeding sessions should not be limited to a predetermined number of minutes dedicated to each breast. Let your baby finish with the first breast before shifting to the other side. This gives the baby the opportunity to receive all the ingredients of high nutritional value required for it to grow. Let your baby breastfeed on the first breast until the intensity of swallowing decreases. When sucking becomes slow change side, and if required, repeat the above process.
Mastitis is a microbial infection of a lobe of the mammary gland. Symptoms usually involve hardening of the infected point, high fever as well as a feeling of fatigue. Following your doctor’s advice, if symptoms persist for more than one day, a treatment shall be administered which shall be compatible to breastfeeding. Note that breastfeeding should not be interrupted due to mastitis.
Learn as much as you can about breastfeeding even before labor. During pregnancy your body is getting ready for breastfeeding whether you are aware of it or not. The hormonal changes taking place in your breast during pregnancy is sufficient preparation for most women. Avoid rubbing your nipples because this practice might possibly harm you, making breastfeeding difficult. The most effective way to avoid pain is for your baby to learn early the correct breastfeeding position. Various products are available to make breastfeeding more comfortable and convenient but their purchase is not required.
Prepare your breast with a hot breast bath or using hot medical dressings and continue with a soft massage following the direction of lactiferous glands to avoid any injury. Avoid using the pump for a long time on the same nipple but just for a few minutes having first prepared the breast in the way described above.
1st stage milks (0-6 months)
Concerning the quality and the quantity of the proteins present in 1st stage milks, they are adjusted to breast milk proteins.
- Contain nucleotides which have been proven to strengthen the infant’s immune system,
- Are digestible and absorbable by the baby’s digestive system due to their lactose content,
- Some of them contain prebiotics or/and probiotics contributing to the intestinal flora balance and to the strengthening of the immune system,
- Are enriched with Polyunsaturated Fatty acids (PUFAs), linoleic and a-linolenic acid (LC-PUFAs), Arachidonic acid (AA), and Docosahexaenoic acid (DHA) contributing to the brain’s proper development and the baby’s vision.
During the first six months of its life, your little baby should be fed exclusively with milk. As of the 6th month onward, the baby has increased needs in calcium, iron and minerals and other types of food should be introduced. Nevertheless, during the 2nd stage, milk is still playing a decisive role in your baby’s nutrition, whether administered by your breast or with the feeding bottle as powdered formula.
Weaning (6-12 months)
Until the 6th month of age, breast milk in itself or in combination with a 1st stage infant formula is sufficient to cover your baby’s nutritional needs. After the 6th month of age, your baby’s increased needs in energy and nutrients are different and the exclusive feeding with milk cannot fully cover these needs for a healthy development. After the 6th month of a baby’s life, the requirements in iron, calcium and vitamins constantly increase.
Therefore, weaning serves various needs such as:
- Coverage of increased energy requirements that would ensure its smooth development,
- Tasting of new types of food, of different texture, taste and flavor,
- Facilitating functions such as chewing and swallowing.
Before the age of 5 – 6 months, babies are in no position to have the required control and coordination of the tongue and mouth muscles. Such acts are necessary for chewing and swallowing. For all above reasons, additional types of food should be added to the baby’s nutrition after the 5th or the 6th month.
With your physician’s consent, you could add:
- From the 6th – 7th month: Rice flour,cream, vegetables (such as carrot, potato, courgette, celery), fruit (such as apple, pear, orange, banana), other cereals, chicken, meat,
- From the 8th – 12th month: Other soft food, such as pasta, cheese, yogurt, beans,
- From the 12th month: Other food.
If breastfeeding your baby is truly not feasible or if your milk is not sufficient, then alternatively you could use the feeding bottle, always following medical advice. If your baby is from 0 to 6 months, then you could administer a 1st stage milk, whereas if it is from 6 to 12 months old, you should administer a 2nd stage milk.
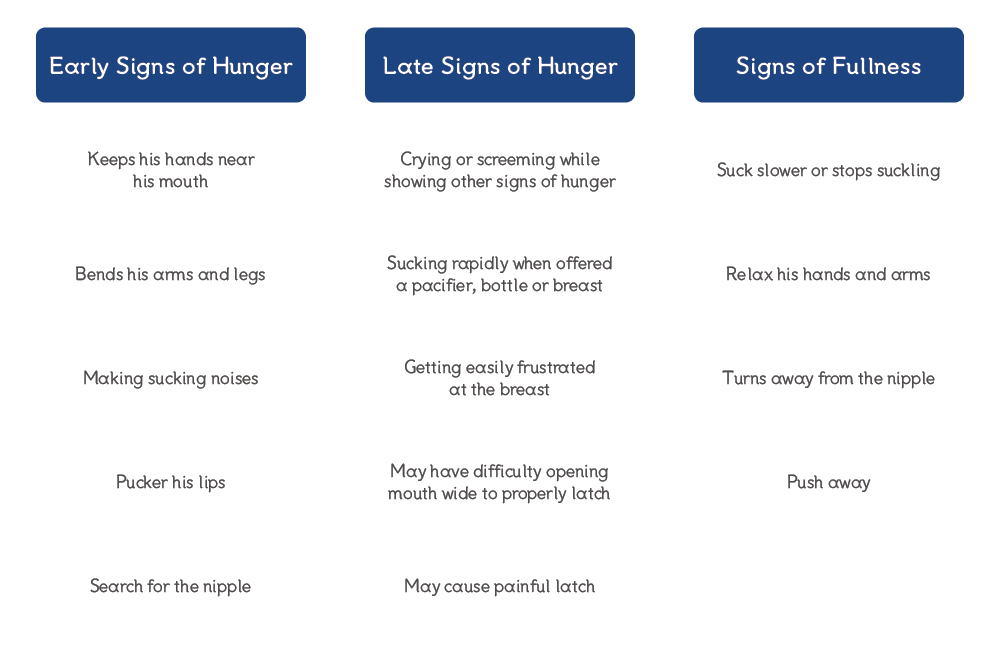
When an infant breastfeeds, we can never be sure of the quantity of milk the baby consumed or whether this is sufficient. Do not worry though because babies have their own way of communicating.
Some of such indications follow below:
- A very important indication of your baby’s saturation is when you see it calm and peaceful after the meal. During breastfeeding, the baby may stop due to fatigue but it could resume breastfeeding afterwards,
- A strong indication is when we see it regaining weight. After the first ten days following childbirth, your baby should be gaining weight,
- After breastfeeding you should feel your breast empty and soft,
- During the first days after birth, your baby should have at least two bowel emptying daily, of yellowish color and the nappies should be wet enough when you change them.
There are however indications that your baby is not sufficiently fed and that it needs more milk.
Such signs could be:
- Various sounds and swallowing sounds during breastfeeding. Probably the baby does not catch your nipple properly,
- One week to ten days after birth the baby’s skin remains yellowish and wrinkled,
- Your baby is nagging and crying immediately after the meal,
- Your baby seems constantly uneasy and tired.
Most of women after pregnancy wish to revert back to their usual body weight before conception, following for that purpose a very rigorous diet. However during breastfeeding, a daily calorie intake of at least 200 calories above the regular calorie intake is required compared to the requirements of a non lactating woman. For this reason milk production is dependent upon the mother’s energy intake.
Moreover, if breastfeeding lasts for more than 3 months or if the lactating woman’s body weight drops below the ideal one for her height, then food-derived energy intake should be accordingly increased. The same happens if the lactating woman breastfeeds more than one infant, as in the case of twins. It is, therefore, recommended during breastfeeding not to aim at body weight loss of more than 2 kilos per month because this will probably result in less milk production.
Diets lower than 1300kcal could negatively affect both milk production and its composition. They should therefore be discouraged.
Βaby

Healthy eating habits begin immediately after birth and are controlled by the parent’s decision on when and how to feed. Parents have a central role in shaping the infant’s feeding and eating habits that are often carried on for the rest of the infant’s life. They usually set priorities and expectations, and provide a role model. They make decisions on the timing and content of the diet, and also on the way in which the infant is fed.
Dietary preferences and even appetite regulation can be affected by the way in which foods are given to the infant, and the interaction between parent and infant.
The feeding relationship is the complex of interactions that take place between the parent and infant as they engage in food selection, ingestion, and regulation behaviors. This relationship thrives when the parent is able to correctly interpret the infant’s feeding cues and abilities, is attentive to the infant’s needs, and responds appropriately to satisfy those needs. The interaction and communication between a caregiver and infant during feeding not only helps the infant to consume a nutritionally adequate diet, but also it influences the infant’s ability to progress in feeding skills. A dysfunctional feeding relationship can result in poor dietary intake and impaired growth for the infant and anxiety and lack of confidence for the parent.
The infant’s health and nutritional status is promoted in a positive feeding relationship (a caregiver that is sensitive and responsive to an infant’s feeding cues and an infant that is fed a nutritionally balanced diet).
A negative relationship (a caregiver consistently misinterpreting, ignoring, or overruling the infant’s feeding cues, e.g. when regularly forces an infant to consume additional food even after he or she has become full and satisfied).
It is increasingly recognized that parenting style can influence the infant’s feeding behavior. An authoritative feeding style (emotionally warm and responsive but with high expectations for children’s dietary quality) accompanied by everyday practices such as modelling consumption of fruit and vegetables, making these foods available within the home, moderately restricting unhealthy alternative snack foods while encouraging children to try fruit and vegetables, is associated with the adoption healthier feeding patterns.
The recognition and response to the infant’s hunger and satiety cues has been gaining attention the last decades because the lack of their recognition and consequently the failure to respond to them has been associated to unbalanced feeding relationship both emotionally and nutritionally. Failing to recognize early hunger cues has been linked to loss of trust in the feeding relationship, hyper feeding and childhood obesity.
| 4 – 7 months |
|
|
| 8 – 12 months |
|
|
– Soothers should not be given to a breastfeeding baby during the first six weeks since birth in order to consolidate breastfeeding.
– The soother should not be offered as a food substitute when the baby is hungry. It may cause strong discomfort and cause problems to its feeding.
– After 2 years of life, efforts should concentrate on the infant’s discontinuing the use of the soother.
Soothers are made of rubber or silicone. Those made of rubber must be replaced when the material starts to stick after frequent use. Soothers made of silicone are softer and the material does not stick after frequent use. However, they present cracks when babies have teeth. Once such cracks are observed in those made of silicone, they should be replaced with new ones.
In infants, the sphincter separating esophagus from the stomach is not sufficiently developed; it is therefore loose pushing stomach liquids upwards to esophagus and then to the mouth, causing regurgitations (‘pouring out’).
Regurgitation is a normal condition; vomiting on the other hand should worry you enough to immediately consult the pediatrician. When regurgitating, the baby ejects a small quantity of milk from its mouth, usually when burping, but it could also happen at any time during the day, even during sleep. When vomiting, the baby throws out a large quantity of milk and is restless.
To reduce regurgitation as much as possible, follow the tips below:
- Feed your baby in a quiet place away from noise,
- Interrupt the feeding session at least once allowing the baby to burp,
- At the end of each session, hold the baby in an upright position in your arms for 5-10 minutes enabling it to burp,
- Avoid feeding the baby when it is lying down
- Refrain from making abrupt movements to your baby after the feeding session,
- If you feed your baby with a feeding bottle, make sure the nipple of the pacifier has the correct size.
If the problem is too intense (the baby frequently pours out long swigs) and it persists for a long time, you should consult a pediatrician or a pediatric gastroenterologist, to help your further investigate the problem.
During a feeding session, make sure the baby is not placed in horizontal position but in a semi-recumbent position and the bottle is parallel to the ground. Try to perceive early the breaks the baby is making while drinking as you should stop feeding if it is choking. When the flow is higher, the baby is forced to swallow faster, so you should modify the flow either making the nipple tighter or using a feeding bottle with a smaller nipple. Take regular breaks to check if the baby is still hungry or if it is well fed.
A hiccup is a normal situation during the first months of a baby’s life and it is common phenomenon particularly after food intake. Hiccups appear a little while after feeding and duration varies from a few minutes up to half an hour. The baby is not disturbed by hiccups but it would be wise to avoid feeding it when hiccup occurs.
The number and texture of poops vary greatly depending on the kind of nutrition and the neonate’s age. Breastfeeding babies poop from 1-7 times per day or even just one poop/week Babies feeding on artificial food poop 2-4 times per day during the first weeks and then have approximately 1-2 poops per day.
Avoid drinking coffee during the entire breastfeeding period. Caffeine passes through breastfeeding to your baby’s body causing irritation. If you definitely need to drink coffee, then do so immediately after breastfeeding, so that your body has the time to eliminate the largest quantity of caffeine until the next breastfeeding.
A burp is caused by swallowing air (aerophagy) during food intake. Babies usually accumulate air while feeding and therefore should be helped to burp, i.e to take the air out of the stomach and then continue their feeding session. At the end of each feeding session, it is always useful to help babies burp, before putting them to sleep. There are many positions that could help the baby burp. The most usual one is to put the baby on the adult’s shoulder with the baby’s stomach on the adult’s chest. Gently pat your baby’s back until it burps. It is not necessary to burp after every feeding session. Therefore, if 5-10 minutes pass without a burp, you can put the baby to the bassinet.
Infantile colic is internationally defined as episodes of unexplained and intense crying in healthy and normally developing babies lasting at least three hours per day, for more than three days a week, at least for three weeks. Colic pains appear during the first 3-4 months of life and unfortunately the causes are unknown.
Breastfeeding, a balanced diet of the mother, a quiet environment and a massage on the baby’s belly can help.
In case of babies presenting colic pains while feeding on formulas and in case the pediatrician ascertains gastroenterological disorders, such as Gastroesophageal reflux, constipation, intolerance to lactose or cow’s milk protein intolerance, powdered milk specially modified to treat colic pains can be chosen following medical advice.
A quiet environment is required during breastfeeding. Make sure you sit comfortably. If you are not using an armchair, put pillows under your elbows. If you had a caesarian section, place the neonate on your side on the pillow to avoid contact with the sensitive section point. During breastfeeding, the entire baby’s body and not only its face should be turned towards facing the breast’s side. Your legs should not be suspended. During breastfeeding, you should allow the air to flow freely from the baby’s nostrils, removing that part of the breast obstructing the nostrils.
Although specialists have diverging views as to the absolutely correct position of neonates and babies, they do however agree that the prone position should be avoided when the baby sleeps unattended. Placing the baby on the prone position has been abandoned in the last 20 years, following an extended campaign as it is blamed as one of the most important causes for the Sudden Infant Death Syndrome-SIDS. The frequency of this syndrome has been mitigated ever since babies do not fall prone for sleep. The babies’ sleep in supine position on a relatively flat and firm mattress is suggested by the American Academy of Pediatrics to avoid as much as possible the sudden death syndrome. Side position can be applied by using a wedge in a relatively firm mattress.